What Is Known About Hypertension
Healthy Steps: Hypertension—First Steps
Healthy Steps: Hypertension—Full Program
You were feeling just fine, not even thinking when the dentist offered to check your blood pressure, obviously not the cause of your visit. Imagine everyone's surprise when the number came out definitely high: 160/100. Not just a little high, but getting into the range of dangerously high. “Oh, wait your cuff must be off. My blood pressure is never that high!”
You check your blood pressure (BP) again with your own cuff, at your doctor's, at the local pharmacy: incredible, it keeps reading high: 150-160/85-105.
“But I can't have high blood pressure; I feel fine!”
The story in the middle may vary, but the last sentence written above is almost always true: blood pressure creeps up without giving the least signal that something is off.
What is Known
Blood pressure is typically measured by applying a cuff or sleeve to the lower part of the upper arm. Tubing within the cuff is connected to a measuring device that can measure how much pressure is required to compress the whole arm enough to shut off the flow in the artery below the cuff, measured in millimeters of mercury. When the artery is fully compressed, that pressure is thought to match the peak pressure occurring with the beat of the heart. That number is the higher number, the upper number in the fraction and is called the systolic pressure. The lower number is the pressure in the artery in the rest phase of the heart beat cycle, the lower number of the fraction, the diastolic pressure.
Before measuring your BP, you should be seated leisurely and peacefully for 5 minutes. Their arm should be held supported (either on a platform or by the measuring person's grasp) at the level of the person's own heart. The cuff is inflated well beyond an anticipated systolic pressure and slowly deflated while the measurer listens with a stethoscope to the artery: the first appearance of the pulse sound is the systolic number, the last heard is the diastolic. It is considered most reliable to measure the blood pressure, wait several minutes and repeat the measurement. If there is a discrepancy, the lower number is probably more representative; it's usually the second reading.
High blood pressure is a risk factor for other forms of cardiovascular disease, such as heart attacks, stroke, kidney failure and diseases of the smaller vessels. Lowering blood pressure, by whatever means, reduces the risks of those secondary illnesses.
The overall frequency of hypertension in all US adults is about 30%. Hypertension is found at fairly equal rates in men and women; rates are higher in African Americans than in Hispanics or non-Hispanic whites. Among that 30%, one out of every five is unaware that they have high blood pressure. Only half of those with hypertension have their blood pressure controlled, or normalized, by some intervention, usually medication. Both disturbing figures are higher among minority groups and others with sub-optimal access to medical care. It is estimated that for every 10% increase in treatment, we might prevent 14,000 deaths per year. (From an economic point of view, think that most of those deaths occur on the public tab when uninsured folks report to the hospital for a critical cardiac event, undergo a lengthy hospitalization, and do not survive. It would obviously be a savings both in human and economic terms for those people to have access to health care.) In a worrisome trend, hypertension is appearing as an increasingly prevalent problem among adolescents and even children, parallel with the increase in obesity and the metabolic syndrome, currently above 3%.
Your physician will start by diagnosing hypertension based on three readings in the hypertensive categories listed below. Sitting at rest for 5 minutes, with your arm elevated to the level of your heart, your blood pressure should be measured twice. The second reading is more reliably representative of your background blood pressure values. The severity of hypertension is graded by somewhat varying scales into the following categories:
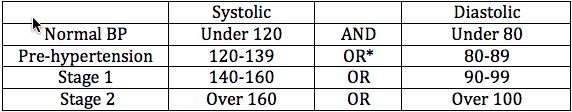
*Among hypertensives, about 65 % have only systolic hypertension, and it may be the most difficult to control. While it was previously thought that diastolic pressures were more predictive, any sustained elevation, of one or both numbers, is cause for intervention. Persistently high pressure, systolic and/or diastolic, raises your risk for heart attacks, strokes and congestive heart failure.
However, it is concluded that about 90-95% of all blood pressure elevation is due to “essential hypertension,” meaning that no cause can be found and easily remedied. I would differ with the use of “essential”, as many non-disease states (such as excessive stress or sleep loss) can elevate blood pressure. In these conditions, high blood pressure typically responds to the suggestions listed below, and you can change your “essential” hypertension to “past history”! After your doctor rules out thyroid and kidney problems, it's your job to walk through the other possible causes of secondary hypertension. Get an upper arm blood pressure monitor that wraps around your upper arm, not your wrist, to monitor your blood pressure at home.
In a conventional medical practice, lifestyle changes (typically weight loss) are typically recommended for pre-hypertension, and medications added for stage 1 and stage 2 hypertension. The medications used to treat hypertension all appear as potential hazards in Dr. David Perlmuttter's The Better Brain Book: The Best Tool for Improving Memory and Sharpness and Preventing Aging of the Brain, and those who take the meds are not surprised. Many of them have either minor or truly annoying side effects, including fatigue, dizziness, lightheadedness, frequent urination, and respiratory irritation. That said, it's obviously safer to have normal blood pressure, and put up with a few side effects, if that's the only way to regulate the numbers!
So let's talk about those lifestyle and nutritional and supplement interventions that have successfully lowered blood pressure in some people. When people normalize what were previously deficiencies (e.g., magnesium, vitamin D) or excesses (e.g., body weight, fasting insulin levels), their blood pressure can also normalize, and their overall health improves. Stressful life situations can swing your body into a chronic state of “sympathetic overdrive”, where the “fight or flight” nervous system is constantly working more than it should. Some of the lifestyle interventions mentioned below can reverse these trends. If such simple interventions can achieve lasting results, that means there are actually fewer cases of “essential” hypertension than previously thought. Rather than hypertension being secondary to renal or thyroid disease, we can see that sometimes it is secondary to lifestyle or other hormonal imbalances. Correcting those imbalances will improve your blood pressure and your overall health.
If you have high blood pressure, I encourage you to read through the information below and see what steps you might take to lower your blood pressure on your own before it stays permanently in the elevated range and you become one more hypertensive patient. Try one or two at a time, stick with the ones that work. If you are already hypertensive, following some of these steps can reduce your need for medication - please consult with your physician about this possibility.
If your blood pressure does not come down with natural means, the safest step to take is to find the minimal dose of the best-tolerated pharmaceutical drug to lower your blood pressure into the normal range. Living with consistently high BP readings is very likely to diminish the quality and length of your life.
Healthy Steps: Hypertension — First Steps
- Reduce your physiological stress messengers by deep breathing, yoga or meditation. Choose one or two of these to do for 15 minutes, once or twice daily.
- Supplement with magnesium. Take Cardiovascular Research Magnesium Taurine daily with meals: take enough to relieve constipation, but not more. In addition, use some form of topical magnesium, either a mineral oil, a mineral lotion, or epsom salts baths. (Epsom salts are also called "Magnesium Sulfate". Choose a form that is acceptable if taken orally, not one that says "Do not take internally.")
- Get at least 7 hours of sleep a night and exercise daily: 5 days a week go for a 30 minute walk and 2 days a week do 15 minutes of High Intensity Interval Exercise, as described in the Lifestyle Section of the Diabetes Health Topic.
Healthy Steps: Hypertension — Full Program
Lifestyle
For hypertension, lifestyle comes first. There have been many studies evaluating different lifestyle changes that have helped some people lower their blood pressure. Not very many people do all of them, but read through the following list, you might be able to manage more of them than you imagine, and even one of them might work for you.
- Lower your insulin levels. Your fasting insulin levels are probably high if you are overweight OR if you have an increase in abdominal fat. You can normalize both your weight and fasting insulin levels by following the Weight Loss Eating Plan or the Paleo Diet. Both eating plans eliminate the refined carbohydrates which can raise insulin and thus serum aldosterone levels, fluid retention and blood pressure. Follow the effectiveness of your eating plan by asking your doctor to check your fasting insulin levels. Ideal fasting insulin is 3-4 uIu/mL, so don't go by the laboratory ranges for normal if you want to reduce elevated BP. (If you reduce your weight by other means - such as calorie counting - the effect on BP is less dramatic and less persistent.)
- Eat Paleo. If you are not overweight, try the Paleo Diet. It has lowered blood pressure in non-overweight individuals.
- Don't smoke. Period.
- Stay active. Gentle aerobic activity (walking, gardening, housecleaning) can help lower blood pressure, and bursts of interval exercise (twice weekly) are the most effective at reducing your risk of a heart attack.
- Drink water. Drink enough water or non-caffeinated coffee and tea: 1/2 an ounce for every pound of your body weight, every day. Adding lemon, ice, or herbs to the water is fine. More water if you're exercising enough to perspire!
- Do some yoga. There is some evidence that regular participation in yoga classes can lower blood pressure, slowly and steadily.
- Take a really deep breath. Alternatively, a good instant relaxer is deep breathing performed in a way to balance what might be an overly stimulated nervous system and elevated blood pressure. Sitting comfortably, take a deep breath. Breathe deeply enough that you feel your lower rib cage expand across your mid back, without raising your shoulders (check in a mirror the first time). Repeat ten times. Take your blood pressure before and after: you'll know right away if this technique works for you. If it does, repeat the ten breaths, three times a day. A gadget called the RESPeRATE
blood pressure lowering device is available for guidance in a well-researched breathing technique. The price tag is significant, so try the method I suggest first!
- Sit in meditation. Medical studies on the benefits of meditation started not long after high-risk personality traits were identified. It seems now that meditation can be helpful across the board, whatever your personality type!
- Avoid lead and cadmium. Toxic exposure to lead and cadmium can raise blood pressure; both usually come from old water pipes, and both should be easily filtered out with the chlorine using a standard water filter.
- Sleep. If you are averaging 5 or less hours of sleep a night, your body responds with stress hormones that raise your blood pressure. Follow the natural measures listed here rather than resorting to anti-histamines or sleeping pills.
- Acupuncture. Preliminary research suggests that acupuncture may prove to be a worthwhile alternative treatment for acupuncture.
Foods to Include
- Follow a Paleo Diet. In recent studies involving both normal and diabetic subjects, the Paleo Diet lowers blood pressure, and improves other metabolic markers, better than the Mediterranean Diet, the current favorite of most practitioners. Both diets outperform the standard American diet, but that's not saying much! (And if someone tells you there is too much red meat or too much saturated fat for your heart, tell them that is an outdated opinion that has been resoundingly reversed.)
- Eat fish twice a week. Emphasize wild caught salmon and other cold-water fish, rich in omega-3 fatty acids, and well-known to be helpful for cardiovascular health, cancer prevention and general reduction of inflammation.
- Nuts! Eat a handful of crispy nuts three times a week!
- Foods rich in Magnesium. Magnesium rich foods can begin to provide the magnesium that most of us are lacking. Focus on dark leafy greens, nuts (again) and seeds, fish, avocados, and a bit of dark (>70%) chocolate, about 100 grams daily seems effective, maybe even less.
- Have salads and raw veggies. Consumption of raw foods might lower diastolic BP. Two generous plates full of salad every day is a great way to eat raw foods. Meat and fish can be eaten raw also, and should be carefully handled.
- Flavor with garlic and onions. Garlic and onions have been folk remedies for hypertension for years. Happily, they make most food taste better: add freely if you enjoy them.
- A small glass of pomegranate juice. Pomegranate juice (naturally low in fructose) consumed daily has lowered some blood pressure significantly, and appears to be a heart-healthy fruit.
- Enjoy dark chocolate! Dark chocolate consumption has been associated with a mild reduction in blood pressure. It is likely that both its magnesium and flavonol content are responsible. To keep quality high and sugar to a minimum, select organic dark chocolate and eat 1-3 ounces daily with meals. One of my favorites is Green & Blacks Dark Chocolate 85% Cocoa.
Foods to Avoid
- Sweets. There is some risk of increased blood pressure with all kinds of sweeteners: sugar, fruit sugar (fructose) and even artificial sweeteners. Fructose is particularly interesting, with recent evidence that one soda a day is enough to double your risk of diabetes. A recent study correlated increased fructose (74 grams daily) in the diet with a significantly increased risk of hypertension. A safe level of consumption is below 25 grams per day: 3-4 pieces of fresh fruit OR less than 1/4 cup of dried fruit OR 1-1/2 cups of orange juice OR 3 cups of pomegranate juice.
- Conventionally raised meat, or CAFO meat. Well, it's not eating the meat - which I would like to say - but rather living near the containment feeding operations that crowds hundreds of animals into dense and unsanitary conditions. The airborne odors raised the blood pressure of neighbors spending time outdoors. Pasture-raised meat is better for blood pressure concerns because of its increased content of omega-3 fatty acids and conjugated linoleic acid, although no focused studies yet have verified a blood pressure effect.
- Coffee and alcohol? Caffeine and alcohol can both increase blood pressure in sensitive people, an effect that should be evaluated on an individual basis.
- Omega-6 rich vegetable oils. Vegetable oils such as soy and canola are fragile, often genetically modified, generally inflammatory and can promote hypertension. Cheap vegetable oils are at their worst as they degrade to hazardous compounds when they are re-used as in deep fryers in fast food restaurants.
Supplements
- Whey protein. Seeming almost too good to be true, research has shown repeatedly that whey protein is a valuable adjunct to any effort to lose body fat, recover from metabolic syndrome, or lower blood pressure and other cardiovascular risk factors. In general, I recommend whey protein as a component of a post-workout smoothie. So on those two occasions a week when you are doing some strenuous exercise, make yourself a whey protein smoothie and consume it within an hour of exercising. I don't recommend more frequent smoothies because of the extra caloric effect of liquid meals, unless one is a vegetarian and relies only on milk, whey, and eggs for protein sources.
- CoQ10. People with hypertension tend to have low CoQ10 levels, and in some uncontrolled studies, supplementation with 30-225 mg/day resulted in significantly lower blood pressure readings, requiring several months for the effect to manifest. Bad news - that's a long wait! Good news - that probably means it's changing something structural, such as the metabolism or physiology of blood vessels. Find a CoQ10 product you can comfortably take for 3-6 months: it will provide other benefits, and that will be sufficient time to see if it will also lower your BP.
- Magnesium. Magnesium can lower blood pressure, particularly if you have any of the other symptoms of magnesium deficiency: muscle cramps, irritability, headaches, palpitations, or constipation. Take enough Cardiovascular Research Magnesium Taurate to relieve constipation, but not more. In addition, use some form of topical magnesium, either a magnesium oil, magnesium lotion, or epsom salts (magnesium sulfate, suitable for oral administration).
- Potassium. Potassium is helpful in many forms that have been shown to lower blood pressure, including 5 servings of fresh fruits and vegetables, potassium supplements and by prescription. Cardiovascular Research Magnesium Taurate has the heart healthy balance of magnesium and taurine; 1-3 daily with meals may be helpful.
- Vitamin D. Optimize vitamin D levels through safe sun exposure (avoid burning, build up your mid-day sun gradually) and supplement as necessary to maintain levels of 40-65 ng/mL.
- Take fish oil. Barlean's Omega 3 Swirl Fish Oil is an excellent source of essential omega-3 fatty acids, vital for cardiovascular health.
- Vitamin C. Credited and accused of almost everything, vitamin C has also been observed to relate inversely to blood pressure: if your vitamin C levels are high, your BP tends to be lower, especially systolic BP. To avoid potential adverse effects, take vitamin C at double the usual recommended daily allowance (see your vitamin C container for specifics).
Controversies
- What about salt? An area of some contention, it has long been thought that modest salt restriction lowered high BP in some individuals, not all. The most recent study noted here observed that low-salt diets were associated with an increased risk of cardiovascular deaths and failed to lower high blood pressure!
- Do we treat all abnormal BP readings? Clearly in some people, chronic pre-hypertension or modest hypertension seems to persist without added risk of other disease. However, most experts agree that once you edge up into the realm of Stage 1 Hypertension, an elevation in one or both of your numbers, your life quality and length will be improved by doing something to make sure your numbers revert to normal.
- What about vegetarians? Although vegetarian diets have reduced blood pressure in some studies, they have no clear advantage over Paleo Diets in that regard, and raise the risk of nutritional deficiencies and other health problems. Vegetarian diets that include eggs and dairy are more likely to be nutritionally complete than vegan diets. Without eggs, vegetarians lack access to the important amino acid taurine.
- Should I take calcium? Although calcium has been shown to lower blood pressure in some studies, it has also been associated with higher rates of cardiovascular disease. If your vitamin D level is high enough, you will absorb all the calcium you need from a well balanced diet.
- Quaker oatmeal? The studies that were done on oatmeal for breakfast compared it to refined grain cereal for breakfast, not to a healthy diet as described in either the Paleo Diet or the Weight Loss Eating Plan. Sneakiness in advertising I'm afraid.
- Soy for heart health? Not in my book: too many risks with soy, including excess estrogen consumption, toxicity to good thyroid health, likely GMO contamination, difficult to digest carbohydrates, and high in the list of potential food allergens.
- B vitamins are more complex. In addition to high BP, elevated homocysteine in the blood is an independent risk factor for cardiovascular disease. I like to see levels below what is normally considered acceptable, hoping for values less than 10 micromoles per liter (mcmol/L). Levels of 10 or high could indicate either a B vitamin deficiency (common in vegetarians and vegans), impaired B vitamin absorption (common in folks over 50 and anyone who has taken a proton pump inhibitor for reflux), or an abnormality in the MTHFR gene, which “helps” your B vitamins do their proper detoxification job with your homocysteine. I'll write a full article on this subject in the future, but for now - discuss with your physician the implications of an elevated homocysteine level
