Building Stronger Bones
What Is Known About Osteoporosis
Healthy Steps: Osteoporosis—First Steps
Healthy Steps: Osteoporosis—Full Program
Preventing Osteoporosis
From Dr. Deborah’s Desk
“It wasn’t even a bad fall, but my wrist just snapped!”
The only good news in that pronouncement was that it was her wrist and not her hip. My new patient, Edith, came to see if there were natural solutions for her recently diagnosed osteoporosis. Her wrist was easily set and recovered about 80% of her pre-fracture strength and mobility. Hip fractures have a much greater impact on quality of life, usually involving a hospitalization, long period of rehabilitation, loss of normal strength and even an increased risk of death.
Edith had been doing as her doctor prescribed: taking a multi-vitamin with the “recommended” amount of vitamin D and supplementing with extra calcium, up to 1200 mg a day. When she drank milk or ate dairy products, she chose low fat dairy and backed off on her calcium. She had never had her vitamin D level tested, but said she still gets out in the sun a bit in the summer time.
Edith is not alone: it is currently estimated that over 200 million people worldwide have osteoporosis and I would venture to say that most of them have received the… “inadequate” advice that Edith had received. A number of them would have actually been tested and started on conventional treatment for osteoporosis: I’m not sure which group is worse off. I have a healthy disrepect for the conventional treatment for osteoporosis, about which I’ll elaborate below.
Throughout our lives our bones undergo a process called “remodeling” in which older bone is re-absorbed and new bone is formed. When we are young children, and adolescents, the process of forming new bone predominates. Through young adulthood, there is a near balance between reabsorption and new bone formation. By the age of 30 we begin to lose bone. In later years as our sex hormones and activity declines, reabsorption predominates, leads to thinning of the bones. Our sex hormones help to keep our bones strong, so as sex hormones decline, so does bone density. For many women, bone loss picks up sharply at menopause; for men, the process is usually more gradual with increased age.
There are many interventions, both natural and pharmaceutical, that can be used to address the increased fracture risk associated with thinning of the bones.
What Is Known About Osteoporosis
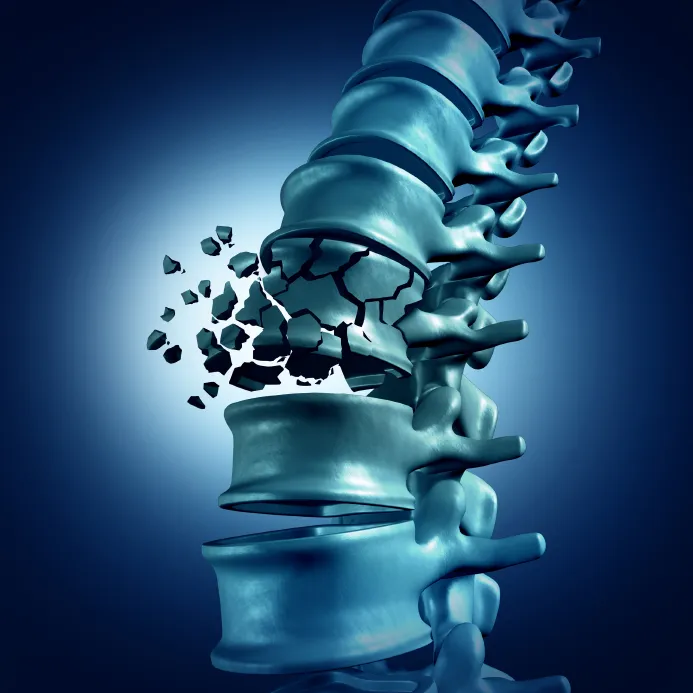
Osteoporosis occurs when the normal process of bone reabsorption becomes more effective than the normal counter process of new bone formation. Bones are weakened and there is an increased risk of francture, especially of the wrist, hip and back. Fractures can occur from minor injuries or seemingly without cause. A vigorous cough can fracture a back bone if osteoporosis has weakened its integrity.
A modest amount of bone thinning occurs almost universally with aging, but many people can maintain effective and strong bones throughout their lifetime. Bone strength is modulated by an interaction of many physiological forces, including systemic hormones, local growth factors, and key nutrients.
- The sex hormones tend to increase bone formation, both testosterone and estrogen. The glucocorticoid hormone cortisol, whether produced internally or taken (as a cortisone pill, shot, cream or inhaled), tends to weaken bones. Parathyroid hormone (from little glands behind the thyroid gland) controls the recycling of bone and high levels of that hormone can increase bone resorption, leading to thinner bones.
- Metabolic status is crucial to bone health: metabolic syndrome and type 2 diabetes are both associated with an increased risk of osteoporosis and osteopenia. Higher insulin levels rather than high sugar levels are associated with lower bone strength.
- The pull of a muscle against the end of a bone stimulates resistance and strengthening of the bone itself. Climbing a flight of stairs or any exercise moving weight against gravity stimulates bone formation. Water exercises, by contrast, elininate the feature of gravity and do not contribute to bone strength. Prolonged bed rest increases your risk for osteoporosis.
- To form new bone, our bodies need a proper combination of vitamin D (to enhance calcium absorption), calcium (although the amount needed is much less than previously thought) and vitamin K2 (to direct our supplies of calcium toward bone formation and away from calcification of non-bone structures).
- Other minor nutrients and lifestyle factors can be influential either directly or by influencing one of the above-listed factors.
Osteoporosis is best assessed through an evaluation of the density of our bones, a bone mineral density evaluation. The gold standard test is called the DEXA or DXA, for Dual X-ray absorptiometry. A special machine uses two x-ray beams, resulting in a very low x-ray exposure, to calibrate the density of the bones of the lower spine and hip, actually the “neck” of the femur or thigh bone. Occasionally the forearm is also or alternatively measured.
Results are compared to what is considered normal bone density, that of a healthy 30 year-old, and are ranked as a T-score. The 30 year old would have a T-score of 0. Extra dense bones have + (positive) T-scores. Thinning bones go into the – (negative) range. Many readings are taken at each site and averaged to yield a total score, one for the back, one for the hip. Readings down to -1.0 are within the range of normal. From -1 to -2.5, the bones are considered “osteopenia”, thinned but not dangerously so. Below -2.5, the bones are considered to be osteoporotic.
There may be no symptoms associated with osteoporosis, or one might notice aching in the lumbar spine, a loss of height (some of this happens in almost everyone, even with good bones), or–worst of all–a broken bone from a minor injury. Broken wrists heal well, but broken back bones often hurt for years, and broken hips require a high degree of medical care, exposing the patient (usually stuck in the hospital for a while) to greatly increased risk of blood clots, pneumonia, and even death. For a woman, a hip fracture raises her risk of dying by 10-20%. The International Osteoporosis Foundation points out that rates of hip fracture vary widely between different populations, higher rates in Scandinavia and North America, lower rates in southern European, Asian and Latin American countries. (Is it the vitamin D? Clearly the more southern countries have greater sunlight exposure, but it’s shocking that such a well-understood vitamin could be significantly deficient in such a large population. Shocking, but not impossible.)
Conventional recommendations and treatment for osteoporosis include some form of vitamin D (often high dose vitamin D2 is recommended), calcium supplementation at the rate of 600-1200 mg. daily, weight-bearing exercise (we agree on this one) and when all else fails, specific medications for osteoporosis.
The bisphosphonate category of meds includes Actonel, Boniva, and Fosamax, all of which interfere with bone resorption, hoping to slow down bone loss. They must be taken correctly to prevent ulceration of the esophagus, and have been observed to cause necrosis (death) of the jaw bone in a small percentage of women.
Evista is a completely different type of medication: it works like an estrogen in the bones, but like an anti-estrogen elsewhere in the body, a twist that is only valuable if you fear the effects of estrogen. It blocks the beneficial effects of estrogens in the mucosa of vagina and urethra, causing dryness, discomfort and potentially increased bladder infections.
Finally, newer medications such as Forteo and Prolia are both given by injection and have not been used for as long.
Happily, there are many natural interventions that can be helpful with the management of osteoporosis. I believe that the most useful approach to preventing and reversing osteoporosis is a comprehensive health program which can improve not just bone density but overall health, and that the pharmaceutical interventions should be reserved for those who do not or cannot comply with the more natural recommendations.
Healthy Steps: Stronger Bones—First Steps
For the greatest health improvement with the fewest steps, do the following:
- Take vitamin D3 in a daily dose taken with meals. You CAN get vitamin D from sun exposure on skin BUT Vitamin D absorption through the skin or GI tract is diminished for people over 50 and for anyone when your shadow is taller than you are. Daily doses should be calibrated to maintain levels of 50-75 ng/mL, or usually 4000 i.u. per day in the northern US, 2-3000 i.u. daily in the southern parts of the US.
- Look for a properly complex Vitamin K. Vitamin K has a value in three different forms: K1, K2 as MK4 and K2 as MK7. My favorite vitamin K that has the proper balance is Thorne Research Vitamin K, take 1 a day. (Others are Jarrow K-Right and K from Life Extension.)
- Supplement also with Creatine Monohydrate 5 grams daily (many brands are fine, I prefer Thorne Research.)
- Stand and walk often throughout your day and follow a weight-bearing or weight-lifting exercise program at least twice weekly.
Healthy Steps: Better Bones—Full Program
A comprehensive program involves many areas in which action steps can be taken, gradually or all at once. You will be your own most valuable health manager. Some of the suggestions below include flexibility: balance gentleness and honesty with yourself!
Start by following the basic nutrition and healthy lifestyle guidelines, with the following modifications:
Savor Helpful Foods
- Protein: Eat to satiety and always accompany with healthy fat to enhance nutrient absorption. Protein helps build stronger muscles which help build stronger bones. Eat protein at every meal, an amount larger than the palm of your hand. Most “elders” do not eat enough. For bone building, animal protein has an advantage over plant protein…. ARE YOU SITTING DOWN? The amount of protein you eat should be 1 gram per pound of your body weight when/if you are lean. Grams of protein, not grams of food. An excellent smart phone App Cronometer can help you count protein,
- Dairy: If you tolerate dairy, it is an excellent source of protein, especially the cultured dairy in cheese, cottage cheese, kefir and yogurt.
- Fat: Essential for nutrient absorption, adequate fat enhances the absorption of the key fat soluble vitamins D and K, as well as the minerals, starting with calcium, that contribute to bone strength. Choose animal fats, healthy oils, avocados, olives and nuts.
- Vegetables: Vegetables provide necessary minerals and phytonutrients. Eat vegetables lightly steamed with butter, cream, and sea salt; or raw in salads with olive oil and vinegar dressing. If you juice your vegetables, drink them with a meal, not instead of a meal, and be sure to retain the pulp with the juice. Butter and oils aid in nutrient absorption. Bitter greens are especially rich in nutrients.
- Fermented foods: Naturally fermented foods enhance digestion and immune function as well as providing valuable vitamin K2. Choose from sauerkraut, kimchi, fermented pickles, cultured vegetables, miso, yogurt, and kefir; eat at the beginning of meals two to three times a day.
- Celtic sea salt: This provides valuable trace minerals, and as insulin levels are lowered, you will excrete increasing levels of salt in your urine. Salt to taste.
- Prunes! By a poorly understood mechanism, dried fruit in general and dried plums, aka prunes, specifically, have a potent effect on reversing bone loss, demonstrated in increased bone density, and increased percentage of weight-bearing trabecular bone.
- Moderate your alcohol. Alcohol interferes with calcium absorption, better less than 1-2 drinks daily.
Avoid Problematic Foods
- Sodas: Never considered a healthy food, sodas of all sorts can interfere with healthy bone physiology.
- Sugar: Limit sugars as needed to keep a healthy weight and metabolism.
- Grains: All grain products (including whole and sprouted grains) may be problematic. Grains interfere with vitamin and mineral absorption and can lead to metabolic syndrome and type 2 diabetes. Gluten in particular may contribute to poor calcium absorption, in the form of celiac disease, with or without a full set of celiac symptoms.
- Alcohol: Avoid excessive alcohol consumption.
- Soy: The only acceptable soy products are fermented tempeh, miso, and tamari. Limit tempeh to one serving per week. Nor is soy an adequate source of protein for your bones: researchers found weaker bones when soy was substituted for meat protein.
- Low-fat, nonfat, or pasteurized dairy products: These highly processed foods do not enhance calcium or vitamin absorption.
Vital Supplements
- Take vitamin D3 in a daily dose taken with meals. You CAN get vitamin D from sun exposure on skin BUT Vitamin D absorption through the skin or GI tract is diminished for people over 50 and for anyone when your shadow is taller than you are. Daily doses should be calibrated to maintain levels of 40-65 ng/mL, or usually 4000 i.u. per day in the northern US, 2-3000 i.u. daily in the southern parts of the US.
- Look for a comples Vitamin K.
- Creatine powder, 5 grams in water every day, is good for building muscles, bones, and brains
- Other valuable supplements include magnesium, omega-3 fish oils, and a good multi-vitamin/mineral supplement.
- NO on Strontium is considered a nutrient, as it appears in tiny amounts in vegetables. Used as a bone-building supplement, high doses are required and may be problematic. Strontium distorts x-rays so makes a DEXA test falsely improved: in fact 75% of an improvement in bone density is artifact due to strontium’s differential response to x-rays compared to calcium. Although largely “safe” in experiments, its infrequent side effects are neurological and in my mind not worth the risk, so I do not recommend it. Strontium is the basis for a drug currently experimental in the US.
- Boron is a nutritional element that may be beneficial for both osteoporosis and osteoarthritis. Boron interacts with copper in building new bone and is probably valuable in the amounts of 2 to 3 mg daily, present in some multi-vitamins, or available as a separate nutrient.
- Calcium is not necessary and may be harmful IF TAKING more than 500 mg daily. Obtain calcium from food, relying on healthy vitamin D levels. Calcium absorption may be impaired in people with celiac disease or those consuming
Lifestyle
- Walking: Discover forms of exercise you love – and do these activities regularly. Brisk walking is sufficient for most people. For even greater benefits, consider adding strength and interval training to a program of daily walking. Walk carefully if you have osteoporosis: you will gradually develop strength and balance, but if you are starting with osteoporosis, you must walk with adequate protection from falling.
- Strength exercises: Working out with weights or even your own body weight (such as performing push-ups), requires intense muscle effort. Weight lifting can be challenging and rewarding: I suggest you work with a trainer to learn proper technique in this form of exercise. Engage in strength training two to three times a week.
- Osteoporosis classes. Many gyms and YMCA’s offer classes particularly designed for people with osteoporosis. If you haven’t done strenuous exercise, it’s great to work with a trainer and/or check out OsteoStrong, a machine-based strengthening program that many people enjoy.
- Caution: Avoid smoking! Smoking can interfere with any bodily function, including the maintenance or formation of healthy bone.
- Caution: Cycling isn’t enough. Even with good physical fitness, cycling does not provide adequate stressors to maintain healthy bone of the spine and hip. It is likely the wrist would be strong in a cyclist, but the most important bones can be weakened from osteoporosis. Cyclists please add weight-bearing exercise, or weight-lifting, to your exercise regimen!
Deep Dive
Ask your health care provider to order key lab tests:
- C-telopeptide measures the rate at which your bones are dis-assembling, ideally
- Procollagen-1-peptide shows the rate of reassembly, ideally > 75
- Vitamin D 50-70
- Fasting insulin > 3 and
Hormone Therapy
For healthy bones it is important to know which hormones to avoid (excessive or unnecessary corticosteroids) as well as to consider which hormones might be helpful. Older men and women both require gender appropriate levels of estrogen (as estradiol) and testosterone to optimize bone maintenance.
Prevention
There is no doubt that making changes in diet and lifestyle can prevent and even reverse osteopenia and osteoporosis. Regular exercise is an important factor in preventing and overcoming osteoporosis. I cannot stress strongly enough how important is some degree of exercise for your bones. Establish the habit of a brisk half-hour daily walk. For even greater benefits, include a moderate program of strength-building exercises and interval training, both of which can dramatically improve your body’s ability to maintain bone strength and even build new bone, at whatever age you are.
From Dr. Deborah’s Desk
I have seen the best benefit from a combined program of smart nutrition and supplementation, weight-bearing exercise and hormone replacement therapy. Both Edith, mentioned above, and a long-time patient, Leslie saw increased bone density with one year of following a combined program. Leslie had developed a parathyroid tumor with high levels of that hormone and serious osteoporosis, quite soon after menopause. For both women, they felt a general improvement from hormone replacement and showed improvement on DEXA scans taken one year apart, following a year of intentional bone-building.
This information is provided for educational purposes only, and any individual diagnosis or treatment should be determined by you and your doctor. See Additional Information.

